Translate this page into:
Low health literacy facts

*Corresponding author: Abdul Kader Mohiuddin, Department of Pharmaceutical Technology, Faculty of Pharmacy, Dhaka University, Dhaka, Bangladesh. trymohi@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Mohiuddin AK. Low health literacy facts. Am J Biopharm Pharm Sci 2023;3:1.
Dear Sir,
Health literacy is strongly associated with patients being able to engage in complex disease management and self-care. The World Health Organization recommends health literacy as an instrument for achieving several key targets listed in the Sustainable Development Goals. People with low health literacy (LHL) may find it challenging to manage their condition and take steps to prevent ill-health, which may lead to increased use of health-care services. Despite the negative implications of LHL, physicians are typically unaware of their patient’s health literacy levels and their subsequent effects on their patients’ outcomes. It affects the use of health services and impacts patient satisfaction and the physician–patient relationship. It is one of the major barriers preventing health-care professionals from adequately transmitting information to people in their care.
Many studies reveal that patients from high-income countries are not adequately adherent to medications as they are prescribed. Forgetfulness, confusion about the duration required for medication use, and mistrust about the overall efficacy of medication are among the reasons for non-adherence to diabetes management protocols in Middle Eastern countries.[1] Conversely, after World War II, Taiwan faced severe poverty which is now the 8th largest economy in Asia and also home of type 2 diabetes patients with more than 80% health literacy.[2] A cross-sectional study of 259 school leaders in Hong Kong, carried out during the COVID-19 pandemic between April 2021 and February 2022 shows that more than 50% of participants had LHL and their LHL was strongly associated with a negative attitude about vaccination, low information, and confusion about COVID-19-related information.[3]
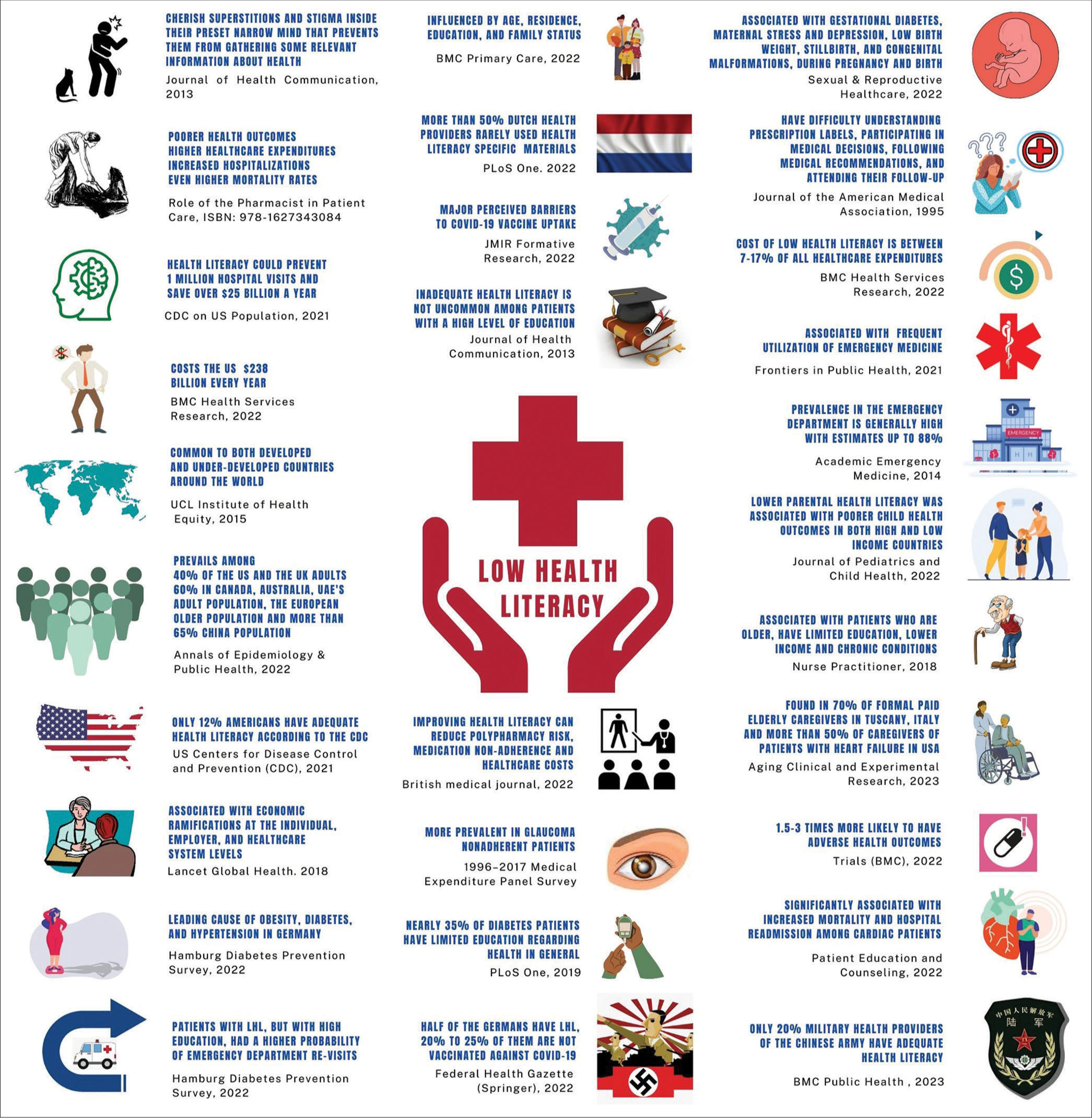
However, in this letter, I would like to present few more sensational facts in the form of an infographic model about LHL [Figure 1]:
LHL is associated mostly with people who cherish superstitions and stigma inside their preset narrow mind that prevents them from gathering some relevant information about health from their surroundings, with a few exceptional cases.[4]
LHL influences a lot of patients’ treatment guideline compliance or more directly medication adherence leads to poorer health outcomes, higher health-care expenditures, increased hospitalizations, and even higher mortality rates.[5]
Only 12% of Americans have adequate health literacy and according to the US Centers for Disease Control and Prevention, improving health literacy could prevent nearly 1 million hospital visits and save over $25 billion a year.[6]
The cost of illiteracy to the global economy is estimated at $1.19 trillion but LHL alone costs the US economy $238 billion every year.[7]
Common to both developed and under-developed countries around the world, socioeconomic conditions are not at all the sole factor of LHL.[8]
Surprisingly, close to 40% of the US and UK adults have LHL, which is around 50% among Europeans; 60% in Canada, Australia, and UAE’s adult population; and close to 70% among the Chinese population.[9]
Health literacy levels increased from 6.48% of the population in 2008 to 23.15% in 2020 in China.[10] However, only 1 in 5 military health providers of the Chinese People’s Liberation Army had adequate health literacy, as found in a recent survey published in BMC Public Health.[11]
Evidence shows that LHL is significantly associated with economic ramifications at the individual, employer, and health-care system levels.[12]
Authors of the Hamburg Diabetes Prevention Survey, a population-based cross-sectional study in Germany concluded that LHL is an important factor in the three conditions of metabolic syndrome-obesity, diabetes, and hypertension.[13]
Health literacy is influenced by age, residence, education, and family status.[14]
More than 50% of Dutch health providers rarely used health literacy-specific materials.[15]
Perceptions of mistrust and LHL were associated with high levels of vaccine hesitancy, providing empirical support for framing these factors as perceived barriers to vaccine uptake.[16]
LHL is not uncommon among patients with a high level of education or with well-off patients. Moreover, patients with LHL, but with high education, had a higher probability of emergency department (ED) re-visits.[7]
Patient-centered interventions have suggested that improving health literacy can reduce polypharmacy risk, medication non-adherence, and health-care costs.[17]
1996–2017 Medical Expenditure Panel Survey by Cheng and Tanna reveals that LHL was more prevalent in patients with glaucoma and patients with LHL were prescribed more medications and had higher medication costs.[18]
Globally, close to 35% of patients with diabetes have limited education regarding health in general.[19]
LHL is associated with gestational diabetes mellitus, maternal stress and depression, low birth weight, stillbirth, and congenital malformations, during pregnancy and birth, with consequences for the woman and her child.[20]
Empirical research on a conceptual model placed the cost of LHL between 7% and 17% of all healthcare expenditures.[7]
In the ED, the prevalence of LHL is wide-ranging, with estimates as high as 88% depending on the ED patient mix and the screening instruments used.[21]
In both low- and high-income countries, lower parental health literacy was associated with poorer child health outcomes.[22]
Associated with older patients, have limited education, lower income, and have chronic conditions.[23]
Was found in more than 70% of formal paid caregivers of not self-supporting older adults in Tuscany, Italy, and more than 50% of caregivers of patients with heart failure in the USA.[24]
People with deficient health literacy may experience 1.5–3 times more serious health outcomes such as higher mortality, hospitalization rates, and inferior disease management ability than those with sufficient health literacy.[25]
Significantly associated with increased mortality and hospital readmission and decreased quality of life among cardiac patients.[26]
Around 50% of Germans have LHL.[27] Every fourth to fifth person in Germany is not vaccinated against COVID-19.[28]
In a 2019 report from Waystar (Health Care Billing Software), close to 40% of health-care consumers stated that they did not know that the cost of their healthcare varied across different facilities.[29]
- Low health literacy facts.
Nevertheless, it can be said beyond reason that health literacy provides a benefit in addressing the health needs of even the most disadvantaged and marginalized communities. To improve adherence, patients need to clearly and appropriately understand health information related to their specific illness or disease. This understanding may be essential to help patients generate the motivation, beliefs, and appropriate health behaviors needed to improve overall adherence behaviors. LHL is a curse, it has to be minimized. All health-care providers, stakeholders, and even government and community authorities should work on it.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Medication adherence: Fact or fictions? Curr Res Public Health. 2022;2:18-21.
- [CrossRef] [Google Scholar]
- Association between health literacy and prevalence of obesity, arterial hypertension, and diabetes mellitus. Int J Environ Res Public Health. 2022;19:9002.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19-related health literacy of school leaders in Hong Kong: A cross-sectional study. Int J Environ Res Public Health. 2022;19:12790.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between health, education, and health literacy: Results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun. 2013;18(Suppl 1):172-84.
- [CrossRef] [PubMed] [Google Scholar]
- Chapter 11. The Enigma of Patient Behavior. The Role of the Pharmacist in Patient Care: Achieving High Quality, Cost-effective and Accessible Healthcare through a Team Based, Patient-centered Approach Irvine: Universal-Publishers; 2020. p. :189-210.
- [Google Scholar]
- Health Literacy Basics-talking Points About Health Literacy. 2021. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/healthliteracy/shareinteract/tellothers.html [Last accessed on 2023 Jan 14]
- [Google Scholar]
- Impact of low health literacy on patients' health outcomes: A multicenter cohort study. BMC Health Serv Res. 2022;22:1148.
- [CrossRef] [PubMed] [Google Scholar]
- Local Action on health Inequalities-improving Health Literacy to Reduce Health Inequalities. 2015. UK Government Publishing Service. Available from: https://assets.publishing.service.gov.uk/media/5a7f46f240f0b6230268e865/4a_Health_Literacy-Full.pdf [Last accessed on 2023 Oct 14]
- [Google Scholar]
- Low health literacy: Treacherous foe of patient compliance in developed countries. Ann Epidemiol Public Health. 2022;5:1097.
- [Google Scholar]
- The development and progress of health literacy in China. Front Public Health. 2022;10:1034907.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of health literacy status and related influencing factors in military health providers of Chinese People's liberation Army, a cross-sectional study. BMC Public Health. 2023;23:4.
- [CrossRef] [PubMed] [Google Scholar]
- High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob Health. 2018;6:e1196-252.
- [CrossRef] [PubMed] [Google Scholar]
- The link between health literacy and three conditions of metabolic syndrome: Obesity, diabetes and hypertension. Diabetes Metab Syndr Obes. 2022;15:1639-50.
- [CrossRef] [PubMed] [Google Scholar]
- Patients' health literacy and health behaviour assessment in primary health care: Evidence from a cross-sectional survey. BMC Prim Care. 2022;23:223.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges and solutions in communication with patients with low health literacy: Perspectives of healthcare providers. PLoS One. 2022;17:e0267782.
- [CrossRef] [PubMed] [Google Scholar]
- Contributions of trustworthiness, health literacy, and self-efficacy in communicating with COVID-19 vaccine-hesitant audiences: Web-based survey study. JMIR Form Res. 2022;6:e38076.
- [CrossRef] [PubMed] [Google Scholar]
- Low health literacy and multiple medications in community-dwelling older adults: A population-based cohort study. BMJ Open. 2022;12:e055117.
- [CrossRef] [PubMed] [Google Scholar]
- Association of health literacy and health care utilization among glaucoma patients. J Glaucoma. 2022;32:139-44.
- [CrossRef] [PubMed] [Google Scholar]
- Correction: Prevalence of limited health literacy among patients with Type 2 diabetes mellitus: A systematic review. PLoS One. 2022;17:e0261430.
- [CrossRef] [PubMed] [Google Scholar]
- Health literacy levels among women in the prenatal period: A systematic review. Sex Reprod Healthc. 2022;34:100796.
- [CrossRef] [PubMed] [Google Scholar]
- Is low health literacy associated with increased emergency department utilization and recidivism? Acad Emerg Med. 2014;21:1109-15.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of parental health literacy on the health outcomes of children with chronic disease globally: A systematic review. J Paediatr Child Health. 2023;59:12-31.
- [CrossRef] [PubMed] [Google Scholar]
- Low health literacy: Implications for managing cardiac patients in practice. Nurse Pract. 2018;43:49-55.
- [CrossRef] [PubMed] [Google Scholar]
- Health literacy of informal caregivers of older adults with dementia: Results from a cross-sectional study conducted in Florence (Italy) Aging Clin Exp Res. 2023;35:61-71.
- [CrossRef] [PubMed] [Google Scholar]
- A behavior change wheel-based interactive pictorial health education program for hypertensive patients with low blood pressure health literacy: Study protocol for a randomized controlled trial. Trials. 2022;23:369.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of health literacy in patients with cardiovascular diseases: A systematic review and meta-analysis. Patient Educ Couns. 2022;105:1793-800.
- [CrossRef] [PubMed] [Google Scholar]
- Health literacy of people with substitutive private health insurance in Germany and their assessment of the health system performance according to health literacy levels: results from a survey. Int J Environ Res Public Health. 2022;19:16711.
- [CrossRef] [PubMed] [Google Scholar]
- Health information behaviour and health literacy on COVID-19 vaccination of the general population in Germany-findings from the CoSiD study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2022;65:1289-98.
- [CrossRef] [PubMed] [Google Scholar]
- Financial health literacy and the shared decision-making process in healthcare. Int J Environ Res Public Health. 2022;19:6510.
- [CrossRef] [PubMed] [Google Scholar]